

Overview
Aquifer Palliative Care provides foundational knowledge and practical clinical application of the principles of palliative care that every clinician should know to improve outcomes and quality of life for seriously ill patients and their families.
Aquifer – supported by the Arthur Vining Davis Foundations – developed a national, standardized curriculum and online course that addresses critical gaps in palliative care learning across undergraduate medical and health professions education.
Aquifer Palliative Care is part of Aquifer’s Clinical Excellence Case Set, which includes 52 cases covering Palliative Care, Trauma Informed Care, Diagnostic Excellence, High Value Care, Social Determinants of Health, and telemedicine.
Why Primary Palliative Care?
Although palliative care is an established specialty, all clinicians should have the skills to provide patient-centered care. This course focuses on primary palliative care, reaching beyond the specialty—moving toward overcoming clinician shortages, lack of access, and lack of training—to teach what every medical and health professions student should know to improve outcomes and quality of life for seriously ill patients and their families.
Vision: Improve the capacity of the US health professions student to deliver humanistic, compassionate interprofessional care centered around patient goals of care and quality of life by applying evidence-based methods to alleviate the suffering of seriously ill patients and their families through the delivery of primary palliative care.
- Part of Aquifer’s Clinical Excellence Case Set, included with Curricular Partner subscriptions and available by subscription to Limited Subscribers
- Designed to equip learners with the knowledge, skills, and attitudes needed to provide patient-centered care to their communities regardless of their future specialty
- Created for educators, by educators, and supported by the Arthur Vining Davis Foundations
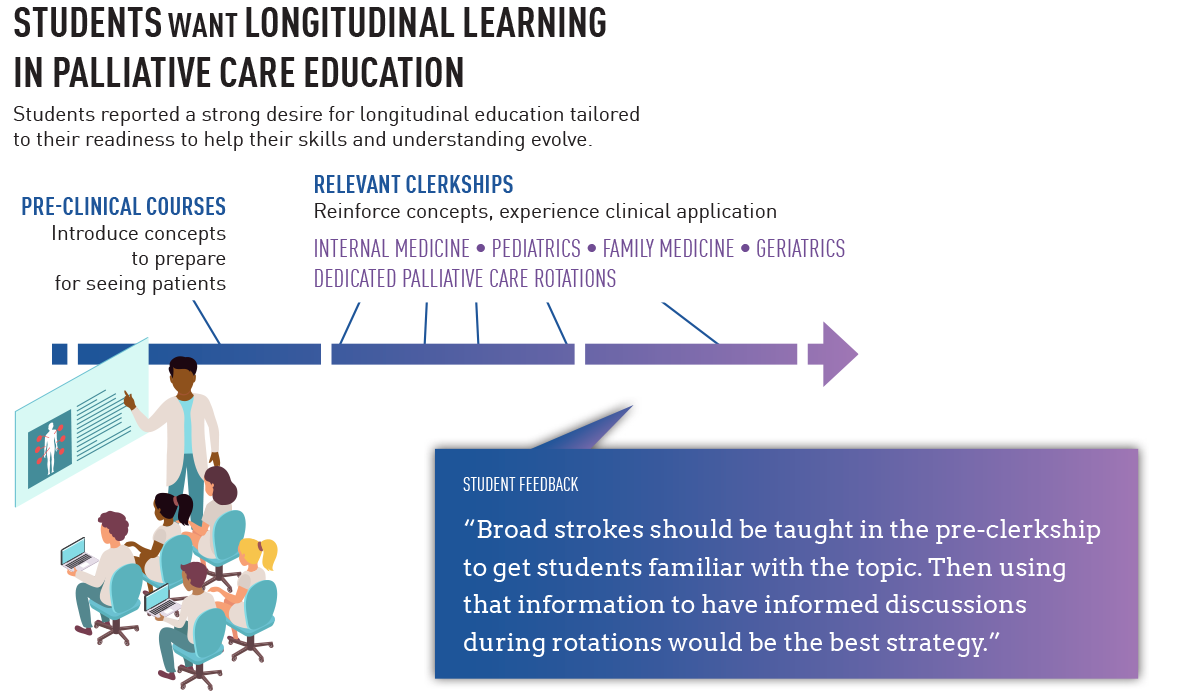
- Ready-made cases to support self-directed learning, appropriate to supplement pre-clinical or clinical learning
- Cases take approximately 15-20 minutes to complete.
- Appropriate to support pre-clinical or clinical learning.
- Can be combined with other cases in a custom course to meet the needs of your specific curriculum.
Based on a comprehensive needs assessment, the Aquifer Palliative Care Leadership Team determined the Principles of Primary Palliative Care Excellence to elevate the primary palliative care education and training of all US health professions students, regardless of discipline. Each principle supports the advancement of primary palliative care as a competency for all healthcare professionals.
- Alignment of care with the goals, values, and preferences of seriously ill patients based on assessed need.
- Interprofessional collaboration and care coordination between patients, families, healthcare teams, and systems.
- Evidence-based and holistic care that addresses the physical, psychological, social, and spiritual domains across the illness trajectory from diagnosis to end-of-life.
- Equitable access to high-quality, culturally sensitive palliative care services for all patient populations.
- Education and advocacy to promote palliative care as a gold standard for serious illness care.
The Aquifer Excellence in Palliative Care cases are designed to teach and apply these principles using clinical scenarios.
After the grant award in 2020 from the Arthur Vining Davis Foundations, Aquifer established a Palliative Care Leadership team, a group of interprofessional clinician-educators and content experts representing schools around the US.
In the absence of clear national curricular standards on palliative care in medical and health professions education, the Leadership Team then completed a needs assessment (stakeholder surveys and focus groups) and literature review. After completing the research activities, the leadership team held a consensus conference, synthesizing the literature review and needs assessment findings into a vision statement and key guiding principles.
Using the vision and principles as a framework, the Leadership Team developed a national palliative care curriculum to be delivered through the Aquifer course. Learning objectives were identified, and development work on virtual patient cases began in late 2021. Case development used varied pedagogies to ensure that learners are equipped with the knowledge, skills, and attitudes needed to provide patient-centered care to their communities.
All Clinical Excellence Case Sets, including Aquifer Palliative Care, now include:
- Principles module: covers key definitions, epidemiology, explanations of key principles and why they are important for patient care, and a harm statement that makes it explicit what harm can come to the patient if the principle is not incorporated into practice.
- Application Cases: Brief, realistic case scenarios that focus on one area of a patient encounter, and are centered around asking students to make important clinical decisions. Content models evidence-based best practices and communication strategies, exploring the real-world impacts on care and potential harm. At the end of each case, a reflection question asks the students to consider key takeaways, implications for their future practice, or personal wellness. Each application case also includes self-assessment questions that extend the learning to other scenarios.
Aquifer Palliative Care is designed for any level student in a medical school or health professions program. The course is an ideal assignment for students to complete as preparation for clinical experiences that include telemedicine. Cases also serve as valuable reference material for students to return to as they need to refresh their knowledge during clinical rotations.
Programs with a current Aquifer subscription will also have faculty and administrator access to an accompanying educator guide. Subscribers will also be able to view student progress reporting and combine the new cases with other Aquifer content in a custom course.
Available to Aquifer Curricular Partners:
- 01: Principles of palliative care
- 02: Palliative care assessment
- 03: Family meetings and establishing goals of care
- 04: Advance care planning
- 05: Interprofessional roles and responsibilities
- 06: Pharmacologic pain management
- 07: Supporting patients and families in the grieving process
- 08: Anxiety and depression in the context of palliative care
- 09: Understanding disparities in care for patients with serious illness
- 10: Non-opioid pain management
- 11: Symptom management (non-pain)
- 12: Pediatric palliative care
- 13: Signs and symptoms of dying
Active Learning Modules
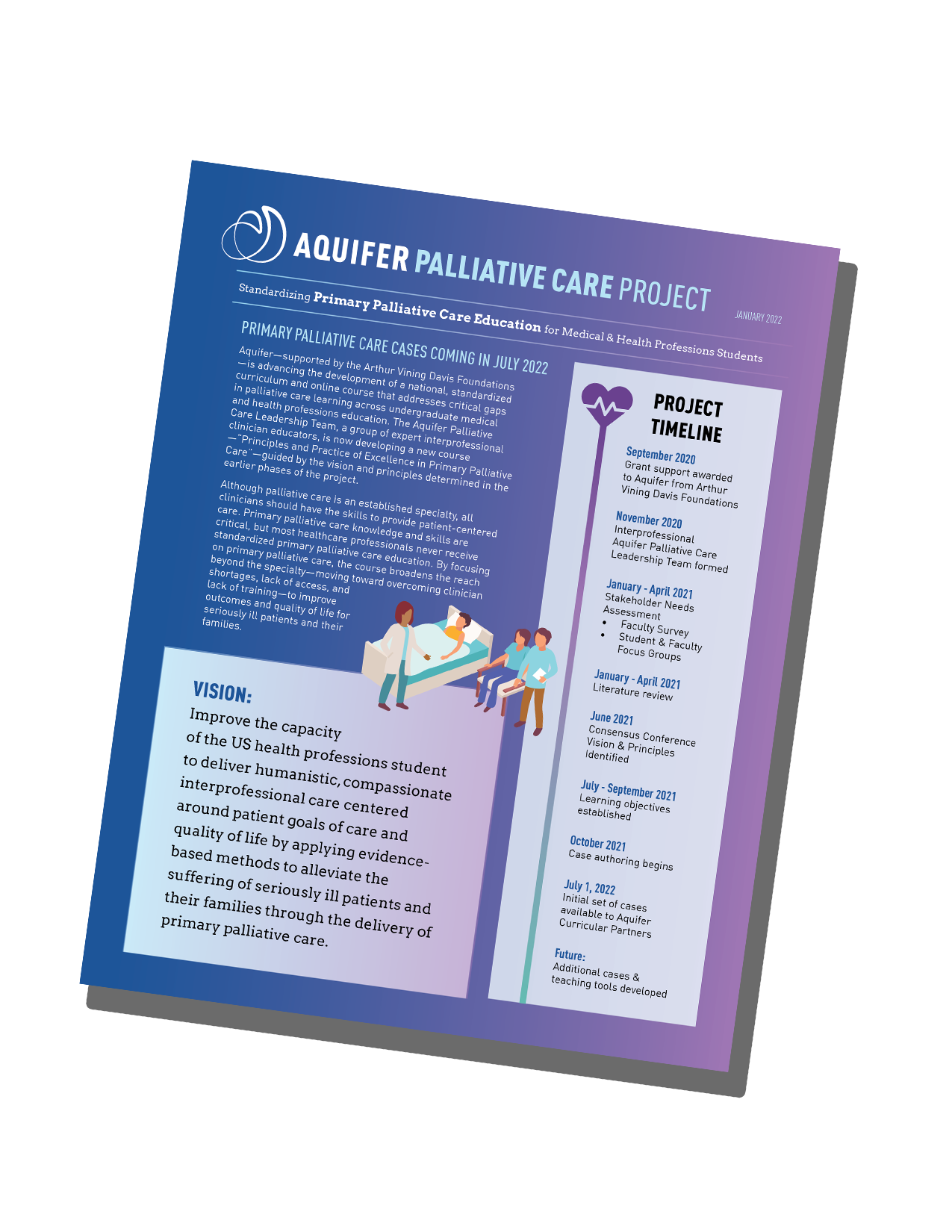
Palliative Care Project Report
Learn More
On-Demand Webinar
Best Practices & New Tools for Teaching What Every Student Needs to Know About Palliative Care
Podcast
Listen to the Aquifer Educator Connection Podcast with April Zehm, MD, as she describes the Aquifer Palliative Care Leadership team’s creation of a national standardized curriculum and soon-to-be-available online palliative care course focused on preparing students to provide high-quality patient-centered care. She also discusses how faculty can integrate course resources into their pre-clinical and clinical teaching.
