By: Vishal Surender, MD | Vice Dean | Windsor University School of Medicine
At Windsor University School of Medicine, we have adopted pieces of our COVID-19 learning design and resources to create a long-term hybrid rotation model with positive student outcomes.
Like many others during COVID-19, we explored ways of engaging students virtually, including using Aquifer across all of our core rotations. As the pandemic continued and rotations resumed in person, the challenge of limited clinical experiences—both due to lack of patient volume and a reduced number of clinical sites—remained for our students. We decided to keep components of our virtual experience and create a long-term hybrid rotation to ensure students met the goals and objectives of the required clinical experiences in a structured way, leveraging the instructional design work and curriculum created at the start of COVID-19.
As we refined our approach to using Aquifer cases, we found success in carefully linking our learning objectives to assessments and focusing on engaging students in a variety of active learning strategies for online active learning in preparation for face-to-face skills sessions. By implementing this approach across all of our clerkships, we saw NBME shelf exam and OSCE scores improve and student confidence rise.
Hybrid Structure Prepares Students for Real Patients
We implemented a hybrid curriculum that involved both traditional teaching methods of incorporating student learning at clinical teaching sites and a new online weekly core curriculum that engaged learners synchronously and asynchronously. The core curriculum covered topics that were considered essential to meet the didactic objectives of the rotation.
By creating an engaging hybrid rotation structure, we are able to better prepare students to succeed in their live clinical application experiences. The online weekly curriculum structure was implemented in conjunction with in-person rotations. For example, for our 6-week OB/GYN clerkship, while students are engaged in their face-to-face rotation experience, students completed 4 weeks of virtual instruction. The initial 2 weeks focused on obstetrics, with 2 later weeks for gynecology, while weeks 3 and 6 were dedicated to assessment. For longer 12-week rotations like Internal Medicine, while students are engaged face to face at clinical sites, they simultaneously engaged in 8 weeks of virtual instruction with topics subdivided into 4 modules (2 weeks each), with one-week assessment breaks in between them. The topics for each week’s virtual curriculum are derived following the order of Aquifer cases or rotation-specific professional organizations. The clinical domain objectives were adopted from Aquifer, which are in line with several core rotation clerkships like COMSEP Curriculum Revision Action Team Toolkit and others, along with our own clerkship-specific objectives.
The hybrid curriculum was created to allow students to gain foundational knowledge and clinical skills, facilitating easier application and solicitation of other competencies while students engage in face-to-face clerkship experience. It was important to make the virtual portion of the rotation simple for faculty to deliver and assess, which we accomplished by using easy-to-use learning platforms like Aquifer and Google Classroom. In addition to Aquifer, we also used internally developed resources and other available cases from APGO, COMSEP, OPENPedeatrics, American College of Surgeons, and AAIM.
Synchronous Sessions: Quizzes & Case Discussions
The key feature of the virtual section of our hybrid learning program was using once a week per rotation synchronous active learning instructional sessions like team-based learning (TBL) and review of pre-assigned case activities from Aquifer. We use the Aquifer Case Analysis Toolkit (CAT) as an active learning tool for students to complete on their own, as well as serving as a basis for in-class discussion, and a graded assignment. The CAT offered an opportunity for our students to refine the important stepwise process that mirrors what clinicians use in evaluating patients in daily practice. This also allowed our preceptors to recognize that student learning, especially at the third-year level, is at a reporter and interpreter stage of RIME framework. We also used the Aquifer Radiology Flipped Classroom Workshops, which include pre-made PowerPoint lectures with notes and questions to engage students.
We used an iRAT (individual readiness assessment) quiz as the first assessment each week, based on the asynchronous assignments. Students were continually assessed using team application exercises, which utilized cases modified and derived from Aquifer and other professional organizations. By combining discussion and assessment, we were able to engage students and ensure that all topics assigned asynchronously were reviewed during synchronous sessions. Cases were discussed by the dedicated clerkship-specific instructors (one each from clinical and pre-clinical phase) by reviewing quizzes, case discussions, and reviewing the CAT.
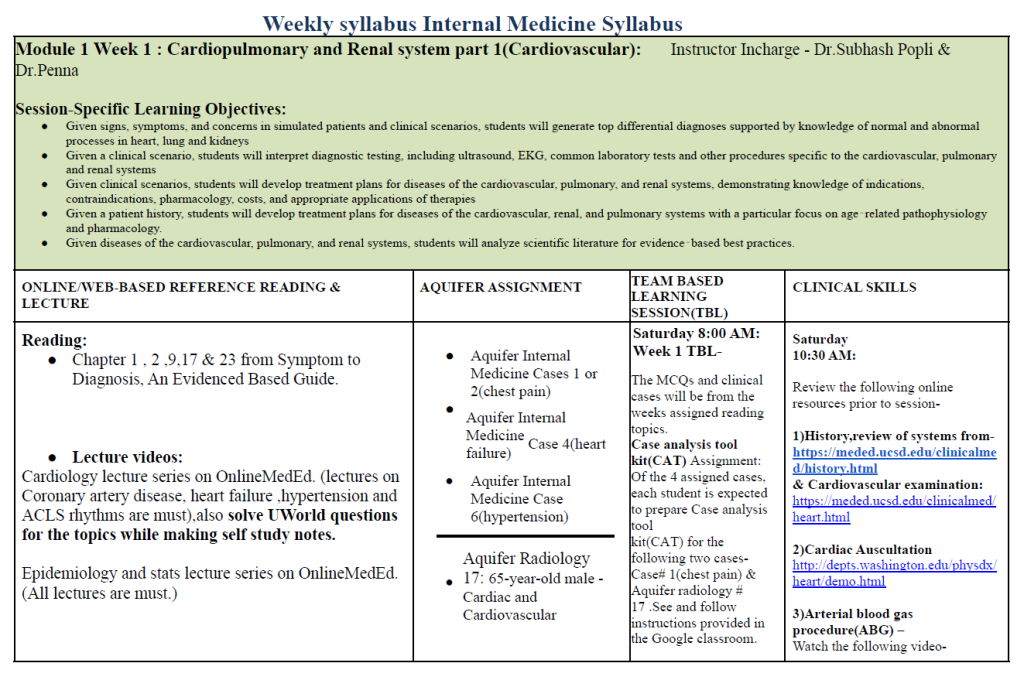
Sample of weekly hybrid curriculum
Assessment Strategies
OSCE’s Based on Aquifer Cases
A key feature for assessments like OSCE in certain clerkship rotations, like pediatrics and internal medicine, was the utilization of Aquifer cases. We used cases from Aquifer that students had not been assigned as a base to modify and create standardized patient-based examinations.
The common clinical skills in each rotation—which were commonly assessed as individual tasks during end rotation OSCE—were made part of each week’s clinical skills training. For example during the obstetrics and gynecology clerkship, one of the OSCE cases dealt with labor and delivery. This particular task was addressed and taught during the OBG week 2 simulation session utilizing Aquifer Family Medicine Case 30 in conjunction with APGO`s basic clinical skills teaching module.
Linking Cases to Assessment
We have closely linked Aquifer cases to our assessment structure, including completion of assignments, participation in the weekly team-based learning session, and the end of rotation OSCE, many of which are structured around Aquifer cases. This strategy has resulted in students engaging with the cases in a more meaningful way. Here is our typical assessment distribution for our hybrid clerkship:
- Completion of Online Assignments (Aquifer & Case Analysis Tool ) – 5%
- Weekly TBL – 15%
- Student Portfolio- Case report, log set & MiniChex-10%
- NBME Shelf Exam – 30%
- Preceptor final evaluation form – 30%
- End of rotation OSCE- 10%
Outcomes: Rising Exam Scores & Confidence
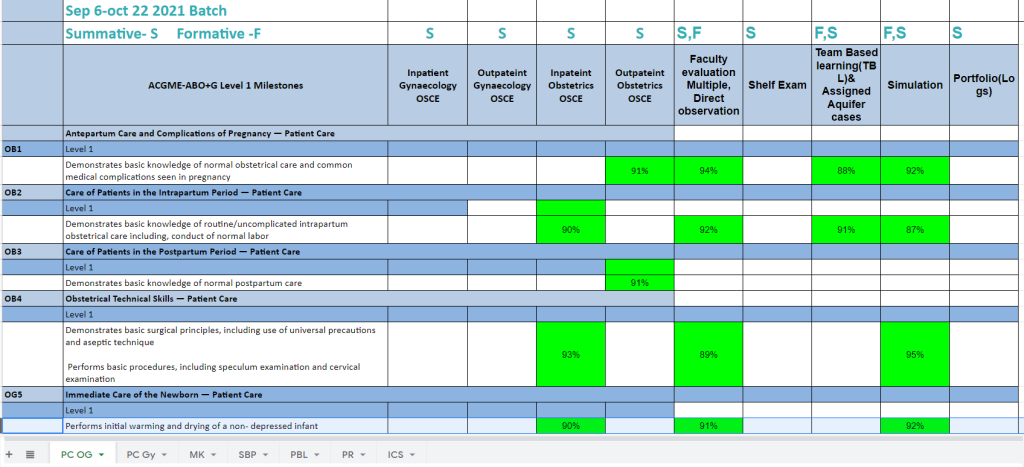
The students have expressed that the hybrid clerkship experience has made them more comfortable and confident in participating in patient care, performing supervised procedural skills, or even doing routine clinical examinations during their actual face-to-face interactions at the clinical teaching sites. They have also expressed that their weekly involvement and following the structured curriculum was a benefit, providing an appropriate foundation and knowledge base to do well in their clerkship. This was corroborated by noticing an improved performance of students in NBME shelf and end of rotation OSCE examinations. We are also confident in preparing the students for their residency training, as students towards the end of each clerkship rotations have shown proficiency in level 1 and in certain cases level 2 of the ACGME milestones and achieving required EPA`s. See table below.
Faculty Feedback & Challenges
The feedback from faculty has also been very encouraging, several of the faculty found this structured approach helpful in terms of gauging students’ knowledge. During actual bedside teaching sessions, faculty feel more able to focus on teaching patient management issues. One challenge we faced is that since not all clinical preceptors participate in the weekly instructional sessions, there was a gap in preceptors being aware of what are the weekly topics assigned to students. Relevant department chairs and clerkship directors have worked on filling this gap. Another challenge is the increased workload on the dedicated instructors, which was heaviest initially when they worked to create CAT answer keys for clerkship rotations (except pediatrics, which has a CAT answer key included from Aquifer).
This hybrid approach, with closer alignment of objectives between instruction and assessment, ensures a better foundation from which students do better during their face-to-face clerkship rotations. We have utilized several resources, but Aquifer came the closest to helping us efficiently address this goal. Other schools can definitely benefit from the usage of readymade educator resources available on Aquifer. Certain innovative tweaking of the Aquifer tools — like usage of cases as a base for creating standardized patients and including a review of the Case Analysis Toolkit during synchronous sessions — aids in closer compliance of students completing the assigned Aquifer cases.