From the American Geriatrics Society:
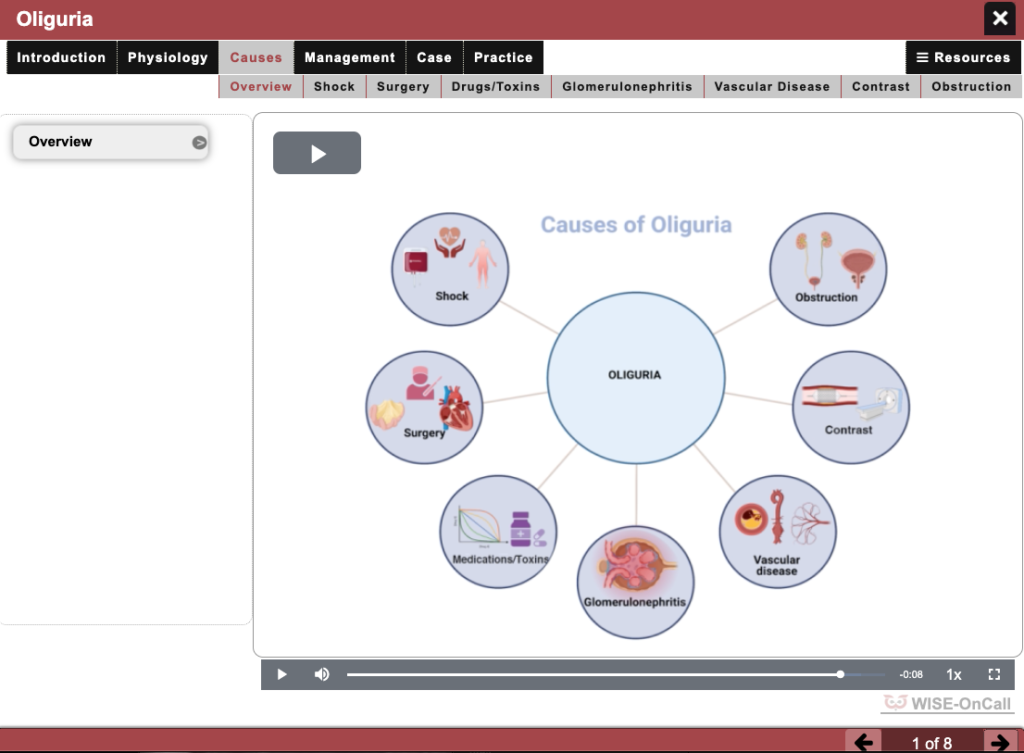
We Need All Health Providers to be Proficient in Geriatrics-Informed Care; A New Online Curriculum Brings Us Closer
- Training all health professionals to care optimally for older adults is critical as we all age; the new @AquiferOrg @AmerGeriatrics online curriculum has solutions to get us closer: http://ow.ly/Wqn130okZ8e
New York (April 5, 2019)—Among many breakthroughs that have made living longer possible, better health care—and more experts to make that care possible—loom large. Given that all of us are aging, we need more clinicians, researchers, and advocates to keep that momentum going. Ideally, for example, we’d already have more than 22,000 geriatricians in the U.S. (though at present less than 7,000 certified clinicians are practicing nationwide). With a limited number of geriatricians, how are we to train the next generation of clinicians to optimally care for older people? A new tool from the American Geriatrics Society (AGS) and Aquifer (the non-profit leader in developing clinical learning tools for health professions education) holds promise for bridging that gap. Aquifer Geriatrics (available at Aquifer.org/Courses/Aquifer-Geriatrics/), the AGS national online curriculum in geriatrics, is leveraging e-learning and geriatrics’ thought-leadership to advance much-needed training to care for older adults.
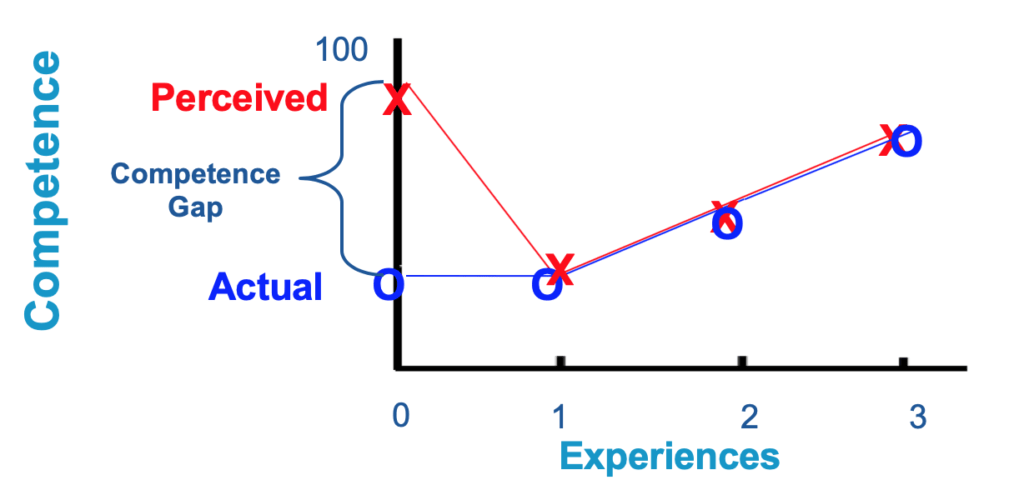
“Almost every health professional in the U.S. will care for older patients at some point in their training or careers,” explains Amit Shah, MD, Associate Dean for Faculty Affairs at the Mayo Clinic Alix School of Medicine, “yet learning about what makes that care unique has varied in duration and even content in the past, often due to a limited number of geriatrics educators at our health professions schools. Developed initially with funding from the Donald W. Reynolds Foundation, the cases that make up Aquifer Geriatrics provide up-to-date, evidence-based content in geriatrics education. They teach healthcare professionals how to appropriately care for older adults, and they make it easy to do so even if a geriatrician is not immediately available to teach some of the basics.”
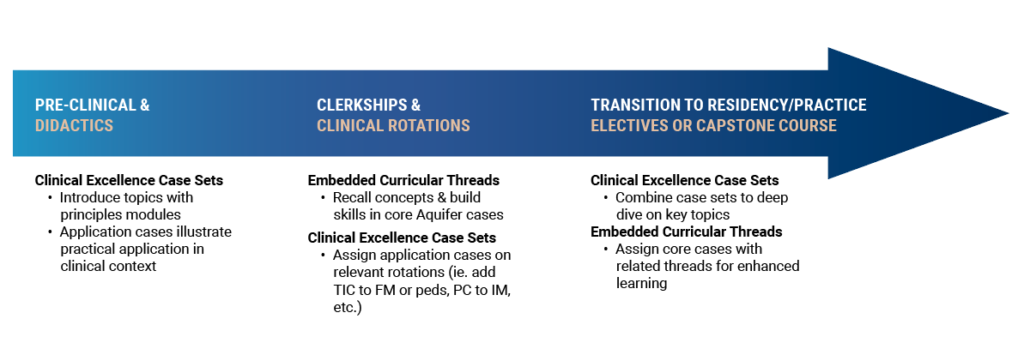
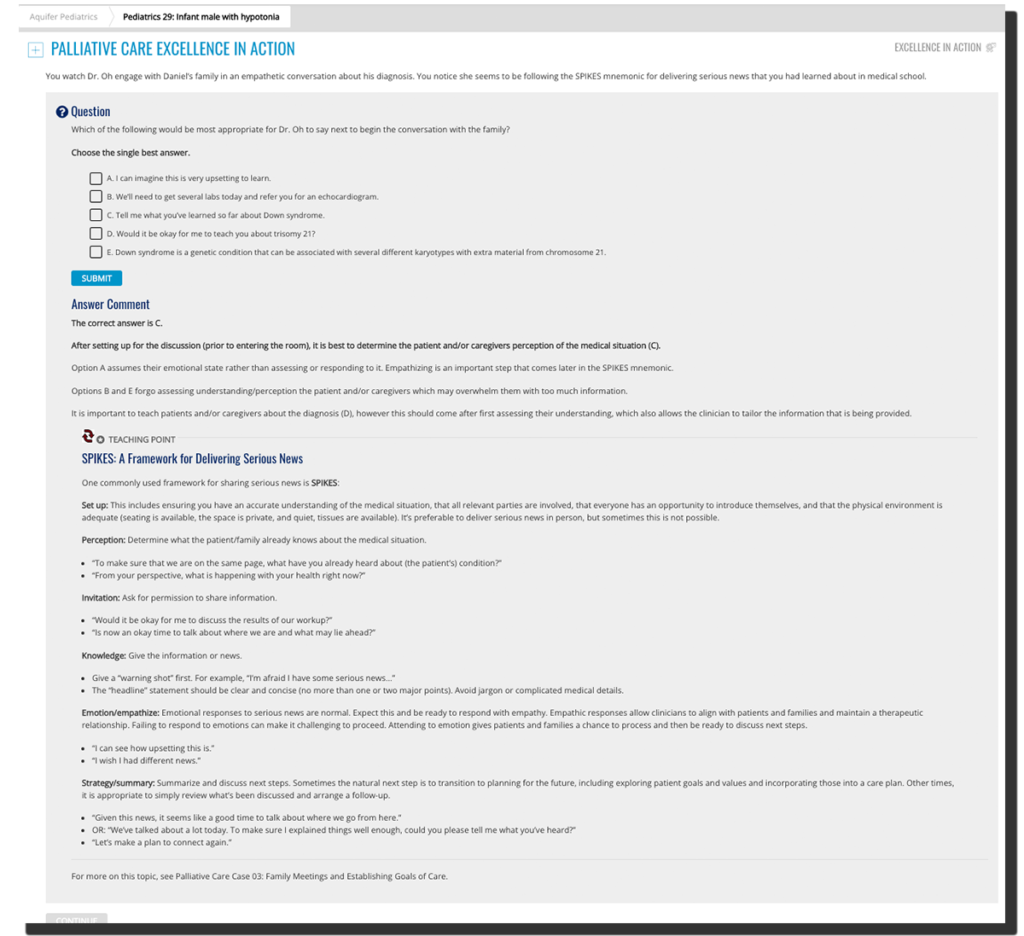
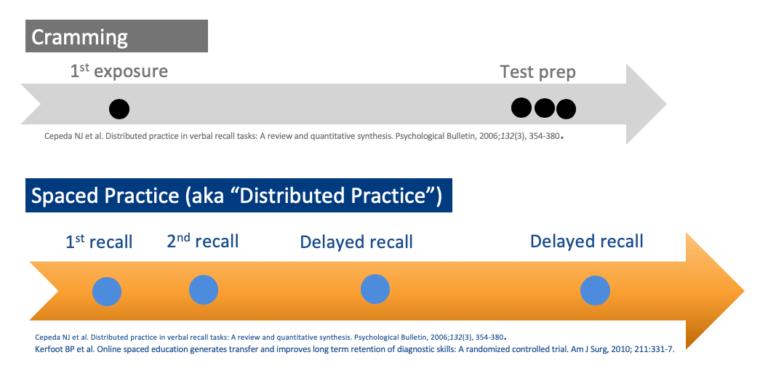
The idea behind Aquifer Geriatrics is simple: Learners at subscribing institutions have instantaneous access to each of 26 evidence-based, peer-reviewed cases addressing the fundamentals of caring for older adults. The Aquifer Geriatrics curriculum was developed by experts from the AGS and Association of Directors of Geriatric Academic Programs (ADGAP) using the framework of the Association of American Medical Colleges (AAMC)/John A. Hartford Foundation Minimum Geriatrics Competencies for Graduating Medical Students. Cases meet the needs of today’s learner as they can be completed at their own pace, without being bound to a traditional “classroom.” Subscriptions ensure that the course will be sustainable, providing consistent funding for operations such as content updates from a dedicated board of top educators, maintenance, and support.
“Each of the 26 cases delivers knowledge and skills, but also models a geriatrics health professional’s approach to care,” Mandi Sehgal, MD, Associate Professor of Geriatric Medicine at Florida Atlantic University Charles E. Schmidt College of Medicine, explains. “Rather than focusing on the myth of ‘one right answer,’ each of the cases teaches clinical reasoning and reflects the nuances of what it takes to do what geriatrics does best: Deliver high quality, person-centered care with a focus on function and quality of life.”
An article published today in the Journal of the American Geriatrics Society (JAGS; DOI:10.1111/jgs.15813) introduces the Aquifer Geriatrics curriculum and walks through several of its early successes, as well as strategies to help clinicians and institutions adopt the platform. In a related editorial also published in JAGS (DOI: 10.1111/jgs.15901), independent educational experts noted that the program holds promise for “helping to fill the gap that is left by the shortage of geriatrics educators” in preparing the field to “play the long game,” thanks to innovative solutions to education.
Aquifer Geriatrics cases can be completed on smartphones, tablets, or computers, and can be used independently or by schools with curricular time available to students. The cases also are appropriate for a host of health professionals, from internal and family medicine residents to physician assistants, nurse practitioners, and geriatrics fellows. For more information or to learn about subscription options, visit Aquifer.org/Courses/Aquifer-Geriatrics/.
About the American Geriatrics Society
Founded in 1942, the American Geriatrics Society (AGS) is a nationwide, not-for-profit society of geriatrics healthcare professionals that has—for more than 75 years—worked to improve the health, independence, and quality of life of older people. Its nearly 6,000 members include geriatricians, geriatric nurses, social workers, family practitioners, physician assistants, pharmacists, and internists. The Society provides leadership to healthcare professionals, policymakers, and the public by implementing and advocating for programs in patient care, research, professional and public education, and public policy. For more information, visit AmericanGeriatrics.org.
About Aquifer
Aquifer, formerly known as MedU, is a unique mission-driven non-profit organization dedicated to delivering the best health care education through collaborative development and research into innovative, high-impact virtual teaching and learning methods. With 12 million virtual patient cases completed since its founding in 2006, Aquifer is the leader in developing clinical learning tools for health professions education.